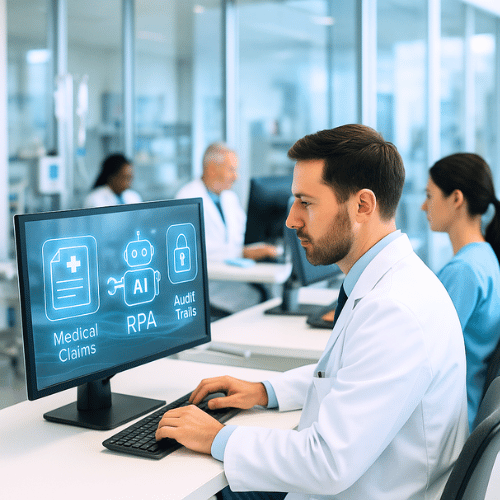
Intelligent Bots to process medical claims
Claim processing is among the most important but time-consuming processes in the healthcare sector. Conventionally, nurses and other healthcare personnel manually gain access to patient files, retrieve information, investigate adherence to protocols, and file claims via government portals. This paperwork not only wastes some precious time, but also poses a risk of human error resulting in reimbursement delays and violations of compliance.
Ramam Tech is an automation company that specializes in Robotic Process Automation (RPA) to automate such repetitive and high-volume processes. Recently, one of our applications was the optimization of the medical claim process for a client who was having difficulties with manual operations. We have replaced the workflow of the clients with an automated, real-time, and error-free system using Dispatcher and Performer bots.
The Problem
The current process of claims used by the client was entirely manual and consisted of a few steps:
Obtaining Patient Records
Employees got into the Client EMR (Electronic Medical Records) System and selected records of specific patients and retrieved important information about them, including the body part, body side, CPT codes, and MTG (Medical Treatment Guidelines).
Confirmation of Reports
It was necessary to confirm the current medical reports of each patient to verify their legitimacy as per the claims requirements.
Government Portal Submission
After the data was verified, the staff used the government portal, input the data that was extracted, filed the claim, and the Claim ID generated by the system was captured.
Employing the EMR System
At last, the personnel returned to the EMR system and revised the identified Claim ID to the patient record and indicated the case as a completed one.
This manual process at the end-to-end was not efficient due to many reasons:
- Time-consuming: It took several logins, extractions of data, and validations to process a single claim.
- Prone to errors: Manual input of the data simultaneously elevated the chances of misaligned information or denied claims.
- Resource-heavy: The skilled employees were wasting their treasured time on low-value repetitive activities rather than attending to the patients or making decisions at the right level.
- Late reimbursement: The lateness or any failure to submit it had a direct impact on the financial cycle of the healthcare provider.
The client wanted an efficient and scalable solution that would decrease the amount of manual intervention, reduce errors, and increase turnaround time.

The Solution
Ramam Tech suggested an automation framework that was RPA-based with a mix of Dispatcher and Performer Bots.
Dispatcher Bot
- Retrieves the patient data (body part, body side, CPT codes, MTG, etc.) and takes it out of the Client EMR System.
- Scans the recent reports to locate possible matches of the claims.
- Enrolls in the Orchestrator Queue all qualified and verified cases to be worked with.
Performer Bot
- Takes out cases one at a time from the Orchestrator Queue.
- Easy access to the government portal.
- Completes the necessary information with a hundred percent accuracy.
- Sends the claim and records the created Claim ID.
- Modifies the Claim ID back to the Client EMR System and closes the record.
This end-to-end automation was well planned, and audit trail, error handling, and exception management were incorporated to comply and provide transparency.
Business Impact
By automating the medical claim process, the following improvements could be measured:
Significant Time Savings
The bots worked through the claims at a speed at least 3 times higher than the human employees. The overall average time to process a client claim was also cut down to a few seconds per record.
Improved Accuracy
The error rates were reduced significantly by abolishing manual data entry. Claims were always made using full and accurate details, which eliminated rejection and resubmission.
Elasticity and Adaptability
The solution was able to deal with workloads that were very different, which could be a few claims per day or even thousands. The supplementary bots can be focused within a short time during the peak season, without the need to hire new staff.
Cost Reduction
The repetitive work was automated, and the staff could concentrate on patient care and other high-value activities. The expense of performing operations through manual claim management has reduced immensely.
Faster Reimbursements
The faster turnaround time meant that claims were approved faster, which had a direct impact on the cash flow of the client.
This design of automation is our line at Ramam Tech, and we have been able to adapt to the industry requirements, designing solutions that are not only technically valid but also industry-specific. For this project, we brought:
- It would entail a lot of knowledge in medical claims.
- Good RPA ability when designing processes to run with more than one bot.
- Secured credentialing and audit trails design.
History of successful implementation of the model that consisted of an unhindered implementation with minimum disruption to the operations.
Why Ramam Tech?